Embarking on the journey of mobility restoration through a total hip prosthesis can be a transformative decision, especially for those living with debilitating joint pain or mobility issues.
Turkey has become a premier destination for orthopedic procedures, attracting patients from around the globe with its skilled surgeons, advanced medical facilities, and significantly lower costs compared to Western countries.
What is a Total Hip Prosthesis procedure?
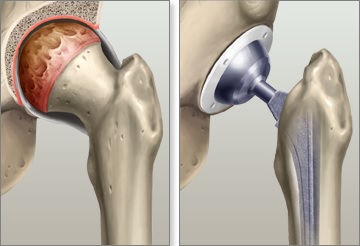
Total Hip Prosthesis involves the surgical removal of the damaged or diseased portions of the hip joint, followed by the implantation of an artificial joint, known as a prosthesis.
The procedure aims to relieve pain, improve mobility, and enhance the overall quality of life for the patient.
Key Components of the Procedure:
- Assessment: The process begins with a thorough evaluation by an orthopedic surgeon, who assesses the patient’s medical history, physical examination, and imaging studies (like X-rays or MRIs) to determine the extent of joint damage and the necessity for a hip replacement.

Who are the best candidates for the procedure?
Severe Hip Pain
The most crucial factor for candidacy is the presence of severe hip pain that interferes with daily activities, such as walking, climbing stairs, or participating in recreational activities. Candidates often experience:
- Chronic pain that persists despite conservative treatments (medication, physical therapy).
- Pain that worsens during movement or at night.
- Pain that limits mobility or leads to difficulty in performing routine tasks.
Degenerative Joint Diseases
Individuals suffering from specific medical conditions that lead to joint degeneration are prime candidates for total hip prosthesis.
These conditions include:
- Osteoarthritis: The most common cause of hip pain, characterized by the wear and tear of cartilage, leading to bone-on-bone contact.
- Rheumatoid Arthritis: An autoimmune condition causing inflammation in the joint lining, leading to joint damage.
- Avascular Necrosis: A condition where blood supply to the hip bone is disrupted, causing bone death and joint collapse.
- Hip Fractures: Severe fractures that cannot be repaired with less invasive methods.
Age and Activity Level
While there is no strict age limit for undergoing a total hip replacement, candidates are typically adults, often in their 50s to 80s.
However, younger patients can also be considered if they exhibit significant hip joint damage and meet the criteria. The following considerations are essential:
- Activity Level: Candidates who lead an active lifestyle or have specific mobility needs often benefit most from surgery, as improved joint function can enhance their quality of life.
- Life Expectancy: Surgeons may consider a candidate’s overall health and expected longevity, as a prosthesis has a lifespan of 10 to 20 years.
Health Status
Candidates should have a comprehensive health evaluation to ensure they can safely undergo surgery. Factors considered include:
- Pre-existing Medical Conditions: Conditions such as diabetes, obesity, or heart disease can affect surgical outcomes and recovery. Proper management of these conditions is essential before considering surgery.
- Overall Fitness: Good physical fitness may improve surgical outcomes and recovery times.
Failure of Conservative Treatments
Candidates for total hip prosthesis typically have not experienced sufficient relief from non-surgical treatment options, which may include:
- Medications (non-steroidal anti-inflammatory drugs, corticosteroids).
- Physical therapy.
- Lifestyle modifications (weight loss, exercise changes).
- Assistive devices (canes, walkers).
Psychological Preparedness
Mental and emotional readiness is an often-overlooked factor in candidacy. Candidates should:
- Understand the procedure, including its risks and benefits.
- Have realistic expectations about post-surgery recovery and outcomes.
- Be motivated to engage in rehabilitation efforts.
Benefits of Total Hip Prosthesis
- Pain Relief: One of the primary benefits of total hip prosthesis is significant pain relief. Most patients experience a marked reduction in hip pain following the surgery, allowing them to resume daily activities without discomfort.
- Improved Mobility: After recovery, patients often notice improved range of motion and overall mobility. This enhancement allows individuals to perform activities such as walking, climbing stairs, and engaging in recreational pursuits more easily.
- Enhanced Quality of Life: With reduced pain and increased mobility, patients typically experience an improved quality of life. They can return to hobbies, exercise, and social activities that may have been limited prior to the surgery.
- Long-lasting Results: Total hip prosthesis can provide long-term benefits, with many patients enjoying relief from symptoms for 10 to 20 years or longer. Modern prosthetic materials and surgical techniques have improved the durability and longevity of hip replacements.
- Restoration of Function: The procedure can restore normal function to the hip joint, allowing patients to regain independence and improve their overall physical activity levels.
Risks of Total Hip Prosthesis
- Surgical Complications: Like any major surgery, total hip replacement carries risks such as bleeding, infection, and adverse reactions to anesthesia. Although these complications are relatively rare, they can occur and may require additional treatment.
- Blood Clots: After surgery, there is a risk of developing blood clots in the legs (deep vein thrombosis) or lungs (pulmonary embolism). Preventative measures, such as medication and physical therapy, are often employed to reduce this risk.
- Prosthesis Failure: In some cases, the artificial hip joint may loosen, wear out, or fail over time, necessitating revision surgery. Factors such as the patient’s weight, activity level, and the prosthetic material can influence the longevity of the implant.
- Dislocation: Dislocation of the prosthetic joint can occur, particularly in the early stages of recovery. This risk is generally higher for certain surgical approaches and may require additional intervention to correct.
- Nerve or Blood Vessel Injury: Although rare, there is a risk of injury to surrounding nerves or blood vessels during surgery. Such injuries can result in numbness, weakness, or other complications.
Factors that influence the price of the Total hip prosthesis procedure in Turkey.
Type of Hospital or Clinic
Public vs. Private Facilities
- Cost Variance: The difference in costs between public and private healthcare institutions can be substantial. Public hospitals typically have lower fees due to government funding, making them more accessible to a wider population. However, patients in public hospitals may encounter longer wait times for surgery and might not receive the same level of amenities or personalized care found in private clinics.
- Service Quality: Private hospitals often provide higher quality services, including more comfortable accommodations, advanced medical technologies, and specialized care. This level of service comes at a premium, which can drive up the costs significantly. Patients may find that the comfort and convenience of a private facility justify the higher price tag.
Reputation and Accreditation
- Accreditation Standards: Hospitals with international accreditation, such as those accredited by the Joint Commission International (JCI), typically adhere to stringent standards of quality and safety. These institutions often charge higher fees due to the investments made in quality assurance and compliance with international healthcare standards.
- Reputation Impact: A facility’s reputation can also affect pricing. Hospitals known for excellence in orthopedic surgery or those with high success rates may charge more due to demand. Patients often prefer well-regarded institutions, which can result in higher costs reflective of the perceived value of care.
Surgeon’s Expertise and Reputation
Experience Level
- Skill and Training: The level of expertise of the orthopedic surgeon performing the total hip replacement is a crucial factor in pricing. Surgeons with extensive experience and specialized training in hip surgeries tend to charge higher fees due to their advanced skill set. These surgeons often have a track record of successful surgeries, which contributes to their higher costs.
- Specialization: Surgeons who focus solely on joint replacements or have completed fellowships in orthopedic surgery may charge more than general orthopedic surgeons. Their specialized training often translates into better outcomes, making their services more valuable.
Success Rates
- Outcomes and Fees: The success rates of surgeons can influence their pricing structure. Surgeons with higher success rates for total hip replacements may command higher fees, reflecting the value they bring in terms of reduced complications and better recovery experiences for patients.
- Patient Satisfaction: Surgeons with strong reputations often have patient testimonials and reviews that reflect their skill and care quality. This positive feedback can drive demand, allowing these surgeons to set higher prices.
Type of Prosthesis Used
Material Choices
- Advanced Materials: The type of materials used in the hip prosthesis can significantly affect costs. Prostheses made from advanced materials, such as ceramic, titanium, or highly cross-linked polyethylene, tend to be more expensive than traditional metal components. These materials are chosen for their durability, longevity, and lower wear rates.
- Durability Considerations: The cost-benefit analysis of using premium materials often favors long-term durability and performance, which can result in lower revision surgery rates in the future. While the initial investment may be higher, patients may save money in the long run by avoiding the need for replacement surgeries.
Custom vs. Standard Prostheses
- Personalized Implants: Custom-made prosthetics tailored to the individual’s anatomical needs may come at a higher cost than standard, off-the-shelf options. Custom implants are designed based on preoperative imaging and planning, ensuring a better fit and potentially enhancing postoperative outcomes.
- Standard Prosthesis Options: Standard implants, while typically less expensive, may not offer the same level of precision and personalization as custom designs. The decision between custom and standard implants can influence overall surgical costs.
Geographic Location
Regional Pricing Differences
- Urban vs. Rural Costs: The cost of living and healthcare in various regions of Turkey can have a significant impact on the price of total hip replacement surgery. Major cities such as Istanbul, Ankara, and Izmir generally have higher healthcare costs due to increased demand for medical services, a larger population base, and higher operational costs for healthcare facilities.
- Access to Specialized Care: In contrast, rural areas may offer lower prices but might lack certain specialized services or advanced medical technologies. Patients in these regions may face longer travel distances for quality care, potentially increasing overall expenses when travel and accommodation costs are considered.
Comprehensive Surgical Packages
Inclusions in Packages
- What’s Covered: Many hospitals and clinics in Turkey offer comprehensive surgical packages that include a variety of services. These packages may cover preoperative assessments, the surgery itself, anesthesia, postoperative care, and rehabilitation services. The comprehensiveness of these packages can significantly influence the overall cost.
- Value of All-Inclusive Packages: Opting for an all-inclusive package can often provide better value for patients. Patients should carefully review what is included in the package to avoid unexpected expenses later. Understanding the details of what the package entails can help ensure that patients receive all necessary services at a transparent price.
Length of Hospital Stay
- Implications for Costs: The duration of hospitalization after surgery is another key factor influencing pricing. Patients who require longer stays due to complications or recovery needs may incur additional costs for room and board, nursing care, and extra medical services.
- Postoperative Monitoring: Extended hospital stays for postoperative monitoring can add to the overall expense, particularly if specialized nursing care or additional treatments are required during recovery.
Preoperative Assessments and Tests
Diagnostic Imaging
- Importance of Imaging: Prior to surgery, patients typically undergo various diagnostic tests to assess the condition of the hip joint. Common imaging studies include X-rays, MRIs, and CT scans. These tests help the surgeon determine the extent of joint damage and inform surgical planning.
- Costs of Diagnostics: The costs associated with these imaging tests can add to the overall price of the procedure. The complexity of the required imaging studies and the facility’s pricing structure can influence these expenses.
Laboratory Tests
- Routine Testing: Routine preoperative laboratory tests, such as blood tests and urinalysis, are essential for assessing the patient’s overall health and suitability for surgery. These tests help identify any underlying conditions that could complicate the procedure.
- Laboratory Fees: The fees for laboratory tests can vary widely depending on the facility and the specific tests required. Patients should consider these costs when budgeting for their surgery.
Anesthesia Costs
Type of Anesthesia
- General vs. Regional: The choice between general anesthesia and regional anesthesia (such as spinal anesthesia) can influence overall costs. General anesthesia generally requires a higher fee due to the involvement of an anesthesiologist, the medications used, and the necessary monitoring during surgery.
- Anesthesia Duration: The duration of anesthesia during surgery may also affect pricing. More complex surgeries requiring longer anesthesia may lead to increased fees, while straightforward procedures may incur lower costs.
Postoperative Care and Rehabilitation
Physical Therapy
- Role of Rehabilitation: Following surgery, patients typically require physical therapy to regain strength, mobility, and function. The cost of these therapy sessions can vary depending on the facility, the therapist’s expertise, and the number of sessions required.
- Duration of Therapy: Patients may need several weeks or months of physical therapy, which can add to the overall expense. Understanding the expected length of rehabilitation can help patients prepare for the associated costs.
Follow-Up Visits
- Importance of Check-Ups: Post-operative follow-up visits with the orthopedic surgeon are crucial for monitoring recovery progress. These visits help ensure that the hip joint is healing properly and that there are no complications.
- Visit Costs: The frequency and costs of these follow-up appointments can vary based on the facility and the surgeon’s practice. Patients should factor in these costs when budgeting for their total hip replacement.
Insurance Coverage
Insurance Policies
- Extent of Coverage: The degree of insurance coverage for total hip prosthesis procedures can significantly impact out-of-pocket expenses. Patients with comprehensive health insurance plans may find that a portion of their surgical costs is covered, while those with limited coverage may face higher personal costs.
- Cost-Sharing Mechanisms: Patients should also be aware of any deductibles, copayments, or coinsurance requirements associated with their insurance policies, as these can further influence the final amount they will pay.
Network Providers
- In-Network vs. Out-of-Network: Patients should check if their insurance network includes the chosen hospital or surgeon. Services provided by out-of-network providers may incur higher costs, potentially leaving patients with significant out-of-pocket expenses.
Complications and Additional Treatments
Surgical Complications
- Potential Complications: Like any major surgery, total hip replacement carries the risk of complications, such as infection, blood clots, or dislocation. If complications arise during or after the procedure, additional treatments or interventions may be necessary, leading to increased costs.
- Management of Complications: Patients who experience complications may require extended hospital stays, additional medications, or even further surgeries, all of which can contribute to rising expenses.
Revision Surgery
- Need for Revision: If the initial hip prosthesis fails or causes complications, revision surgery may be necessary. This additional procedure typically involves higher costs related to surgery, hospital stay, and rehabilitation.
- Long-Term Cost Considerations: While the upfront cost of total hip replacement may seem significant, patients should also consider the long-term financial implications of potential revision surgeries and the durability of the prosthetic implant.
Prices of all types of the Total hip prosthesis procedure in Turkey.
Total Hip Replacement (THR)
Definition and Details:
Total Hip Replacement (THR) is a surgical procedure that involves completely removing the damaged or arthritic components of the hip joint and replacing them with artificial implants.
This surgery is typically recommended for patients with severe hip arthritis, avascular necrosis, or hip fractures, aiming to relieve pain, improve function, and enhance the overall quality of life.
The procedure requires the removal of the femoral head (the ball) and the acetabulum (the socket), followed by the insertion of prosthetic components made from materials such as metal, ceramic, or polyethylene.
The surgery is usually performed under general or spinal anesthesia and can take about 1-2 hours. Recovery times vary but typically involve a hospital stay of 1-3 days and a gradual return to normal activities over 3-6 months.
Procedure Steps:
- Preoperative Assessment: Comprehensive evaluation of medical history and physical examination; imaging studies (X-rays, MRI, or CT scans) are performed to assess hip joint condition.
- Anesthesia Administration: Administration of either general anesthesia or spinal anesthesia based on the patient’s health and surgical preference.
- Incision and Exposure: A surgical incision is made over the hip to access the joint.
- Removal of Damaged Joint: The damaged femoral head and acetabulum are carefully excised.
- Implantation of Prosthesis: The prosthetic acetabulum is fitted into the pelvic bone; the femoral stem is inserted into the femur, followed by the attachment of the artificial femoral head.
- Closure of the Incision: The surgical site is closed using sutures or staples.
- Postoperative Recovery: Monitoring in the recovery room; initiation of physical therapy to encourage mobility.
Pricing Breakdown:
Preoperative Assessments:
- X-rays: $100 – $300
- MRI or CT scans (if needed): $500 – $1,200
- Blood tests: $100 – $200
Surgical Costs:
- Surgeon’s fee: $1,500 – $3,000
- Anesthesiologist’s fee: $500 – $1,000
- Total hip prosthesis implant: $3,000 – $7,000
Hospitalization:
- Daily hospital stay: $500 – $1,500 per day (typically 2-3 days)
- Nursing care and monitoring: $200 – $400 per day
Rehabilitation:
- Physical therapy sessions: $50 – $150 per session (usually 5-10 sessions)
Partial Hip Replacement (Hip Hemiarthroplasty)
Definition and Details:
Partial Hip Replacement, or Hemiarthroplasty, involves replacing only the femoral head while preserving the acetabulum.
This procedure is commonly recommended for older patients with hip fractures or those who may not be suitable candidates for total hip replacement due to other health issues.
Hemiarthroplasty aims to relieve pain and restore mobility while maintaining some natural bone structure.
The surgery is typically less invasive than total hip replacement, leading to shorter recovery times, although it may not provide the same level of stability and longevity as a total replacement.
Procedure Steps:
- Preoperative Assessment: Comprehensive evaluation and imaging studies to determine the extent of damage.
- Anesthesia Administration: Either general or regional anesthesia is administered.
- Incision and Exposure: A smaller incision is made to access the hip joint.
- Removal of the Femoral Head: The damaged femoral head is excised.
- Insertion of Prosthetic Head: The artificial femoral head is inserted into the remaining femur.
- Closure of the Incision: The surgical site is closed with sutures or staples.
- Postoperative Recovery: Monitoring and initiation of physical therapy.
Pricing Breakdown:
Preoperative Assessments:
- X-rays: $100 – $300
- MRI (if needed): $500 – $1,200
- Blood tests: $100 – $200
Surgical Costs:
- Surgeon’s fee: $1,200 – $2,500
- Anesthesiologist’s fee: $400 – $800
- Partial hip prosthesis implant: $2,500 – $5,000
Hospitalization:
- Daily hospital stay: $400 – $1,200 per day (typically 1-2 days)
- Nursing care and monitoring: $150 – $350 per day
Rehabilitation:
- Physical therapy sessions: $40 – $120 per session (usually 4-8 sessions)
Anterior Approach Total Hip Replacement
Definition and Details:
The Anterior Approach Total Hip Replacement is a minimally invasive surgical technique that accesses the hip joint from the front rather than the side or back.
This approach minimizes muscle disruption, which can lead to less postoperative pain and a quicker recovery.
It is particularly beneficial for patients with a lower body mass index (BMI) or those who are relatively young and active.
Surgeons often prefer this method due to its potential for better visibility and control during the procedure.
Patients typically experience shorter hospital stays and a faster return to normal activities compared to traditional posterior or lateral approaches.
Procedure Steps:
- Preoperative Assessment: Evaluation of the patient’s hip condition through imaging and physical examinations.
- Anesthesia Administration: General or regional anesthesia is administered.
- Incision and Exposure: A small incision is made on the front of the hip, allowing access to the joint.
- Displacement of Muscles: Muscles surrounding the hip are gently moved aside rather than cut, preserving more soft tissue.
- Removal of Damaged Joint: The damaged femoral head and acetabulum are removed.
- Insertion of Prosthesis: The artificial components are implanted similarly to traditional approaches.
- Closure of the Incision: The incision is closed with sutures or staples.
- Postoperative Recovery: Monitoring and initiation of physical therapy.
Pricing Breakdown:
Preoperative Assessments:
- X-rays: $100 – $300
- MRI (if needed): $500 – $1,200
- Blood tests: $100 – $200
Surgical Costs:
- Surgeon’s fee: $2,000 – $4,000
- Anesthesiologist’s fee: $600 – $1,200
- Anterior approach prosthesis implant: $4,000 – $8,000
Hospitalization:
- Daily hospital stay: $600 – $1,800 per day (typically 1-2 days)
- Nursing care and monitoring: $200 – $500 per day
Rehabilitation:
- Physical therapy sessions: $50 – $150 per session (usually 5-10 sessions)
Posterior Approach Total Hip Replacement
Definition and Details:
The Posterior Approach Total Hip Replacement is one of the most common techniques for performing hip replacement surgery.
This approach involves making an incision on the back side of the hip, allowing access to the joint by cutting through the gluteus maximus and smaller muscles. It is particularly suitable for patients with significant arthritis or other joint deformities.
While this method provides excellent visualization of the hip joint, it may lead to a slightly longer recovery time due to the muscle disruption involved.
Procedure Steps:
- Preoperative Assessment: Comprehensive medical evaluation and imaging studies.
- Anesthesia Administration: General or regional anesthesia is used.
- Incision and Exposure: An incision is made on the posterior side of the hip.
- Muscle Disruption: The gluteus maximus and other muscles are cut to access the hip joint.
- Removal of Damaged Joint: The femoral head and acetabulum are excised.
- Insertion of Prosthesis: The artificial components are implanted into the hip joint.
- Closure of the Incision: The incision is closed with sutures or staples.
- Postoperative Recovery: Monitoring and initiation of physical therapy.
Pricing Breakdown:
Preoperative Assessments:
- X-rays: $100 – $300
- MRI (if needed): $500 – $1,200
- Blood tests: $100 – $200
Surgical Costs:
- Surgeon’s fee: $1,800 – $3,500
- Anesthesiologist’s fee: $500 – $1,000
- Posterior approach prosthesis implant: $3,500 – $7,000
Hospitalization:
- Daily hospital stay: $500 – $1,500 per day (typically 2-3 days)
- Nursing care and monitoring: $200 – $400 per day
Rehabilitation:
- Physical therapy sessions: $50 – $150 per session (usually 5-10 sessions)
Minimally Invasive Total Hip Replacement
Definition and Details:
Minimally Invasive Total Hip Replacement (MI-THR) is a technique designed to reduce tissue damage during hip replacement surgery.
This approach uses smaller incisions and less muscle disruption, leading to reduced postoperative pain, shorter hospital stays, and quicker recovery times.
Patients who are good candidates for MI-THR often experience better outcomes, including improved mobility and decreased rehabilitation times. Surgeons must be specially trained to perform this technique effectively.
Procedure Steps:
- Preoperative Assessment: Evaluation of the patient’s overall health and hip condition.
- Anesthesia Administration: General or spinal anesthesia is administered.
- Incision and Exposure: One or two small incisions are made to access the hip joint.
- Insertion of Specialized Instruments: Minimally invasive instruments are used to perform the surgery.
- Removal of Damaged Joint: The damaged femoral head and acetabulum are removed.
- Insertion of Prosthesis: The artificial components are implanted using the minimally invasive technique.
- Closure of the Incision: The incision is closed with sutures or staples.
- Postoperative Recovery: Monitoring and initiation of physical therapy.
Pricing Breakdown:
Preoperative Assessments:
- X-rays: $100 – $300
- MRI (if needed): $500 – $1,200
- Blood tests: $100 – $200
Surgical Costs:
- Surgeon’s fee: $2,500 – $4,500
- Anesthesiologist’s fee: $600 – $1,200
- Minimally invasive prosthesis implant: $4,000 – $9,000
Hospitalization:
- Daily hospital stay: $600 – $1,800 per day (typically 1-2 days)
- Nursing care and monitoring: $200 – $500 per day
Rehabilitation:
- Physical therapy sessions: $50 – $150 per session (usually 5-10 sessions)
Dual Mobility Hip Replacement
Definition and Details:
Dual Mobility Hip Replacement is an innovative surgical technique designed to enhance stability and reduce the risk of dislocation following hip replacement surgery.
This approach involves a unique prosthesis design that features an inner and outer socket, allowing for greater range of motion while maintaining joint stability.
It is particularly beneficial for younger, more active patients or those with a history of hip dislocations. The dual mobility system provides improved functionality and reduces the need for revision surgeries.
Procedure Steps:
- Preoperative Assessment: Detailed evaluation and imaging studies of the hip joint.
- Anesthesia Administration: General or regional anesthesia is administered.
- Incision and Exposure: A surgical incision is made to access the hip joint.
- Removal of Damaged Joint: The damaged femoral head and acetabulum are removed.
- Insertion of Dual Mobility Prosthesis: The dual mobility components are implanted.
- Closure of the Incision: The incision is closed with sutures or staples.
- Postoperative Recovery: Monitoring and initiation of physical therapy.
Pricing Breakdown:
Preoperative Assessments:
- X-rays: $100 – $300
- MRI (if needed): $500 – $1,200
- Blood tests: $100 – $200
Surgical Costs:
- Surgeon’s fee: $2,000 – $4,000
- Anesthesiologist’s fee: $600 – $1,200
- Dual mobility prosthesis implant: $5,000 – $10,000
Hospitalization:
- Daily hospital stay: $600 – $1,800 per day (typically 1-3 days)
- Nursing care and monitoring: $200 – $500 per day
Rehabilitation:
- Physical therapy sessions: $50 – $150 per session (usually 5-10 sessions)
Resurfacing Hip Replacement
Definition and Details:
Resurfacing Hip Replacement is a less invasive alternative to traditional hip replacement surgery, primarily designed for younger patients with hip arthritis.
This technique involves capping the femoral head with a smooth metal surface instead of removing it entirely.
The acetabulum is also prepared to receive a metal socket. Resurfacing preserves more of the patient’s natural bone structure and often results in quicker recovery times. However, it may not be suitable for all patients, particularly those with significant bone loss or specific medical conditions.
Procedure Steps:
- Preoperative Assessment: Evaluation of the hip condition and imaging studies.
- Anesthesia Administration: General or spinal anesthesia is administered.
- Incision and Exposure: A surgical incision is made to access the hip joint.
- Preparation of Femoral Head: The femoral head is prepared for capping.
- Insertion of Resurfacing Prosthesis: The metal cap is fitted onto the femoral head, and a new socket is implanted into the acetabulum.
- Closure of the Incision: The incision is closed with sutures or staples.
- Postoperative Recovery: Monitoring and initiation of physical therapy.
Pricing Breakdown:
Preoperative Assessments:
- X-rays: $100 – $300
- MRI (if needed): $500 – $1,200
- Blood tests: $100 – $200
Surgical Costs:
- Surgeon’s fee: $1,800 – $3,500
- Anesthesiologist’s fee: $500 – $1,000
- Resurfacing prosthesis implant: $3,000 – $7,000
Hospitalization:
- Daily hospital stay: $500 – $1,500 per day (typically 1-2 days)
- Nursing care and monitoring: $200 – $400 per day
Rehabilitation:
- Physical therapy sessions: $50 – $150 per session (usually 5-10 sessions)
Revision Hip Replacement
Definition and Details:
Revision Hip Replacement is a surgical procedure performed to replace or repair a previously implanted hip prosthesis.
This surgery is typically indicated for patients who experience complications such as implant loosening, infection, dislocation, or wear and tear of the prosthetic components.
Revision surgeries are generally more complex than primary hip replacements and may involve additional challenges related to bone loss or scarring from previous surgeries.
Procedure Steps:
- Preoperative Assessment: Comprehensive evaluation of the patient’s hip condition and previous surgeries.
- Anesthesia Administration: General or regional anesthesia is administered.
- Incision and Exposure: An incision is made to access the previously implanted hip joint.
- Removal of Old Prosthesis: The existing implant is carefully removed, taking care to preserve surrounding bone and tissue.
- Preparation of Bone: Assessment and preparation of the bone for the new prosthesis; may involve the use of bone grafts if significant loss is present.
- Insertion of New Prosthesis: The new hip implant is inserted, which may include the use of larger or specially designed components to accommodate bone loss.
- Closure of the Incision: The incision is closed with sutures or staples.
- Postoperative Recovery: Monitoring and initiation of physical therapy.
Pricing Breakdown:
Preoperative Assessments:
- X-rays: $100 – $300
- MRI (if needed): $500 – $1,200
- Blood tests: $100 – $200
Surgical Costs:
- Surgeon’s fee: $2,500 – $5,000
- Anesthesiologist’s fee: $600 – $1,200
- Revision prosthesis implant: $4,000 – $9,000
Hospitalization:
- Daily hospital stay: $600 – $1,800 per day (typically 2-4 days)
- Nursing care and monitoring: $200 – $500 per day
Rehabilitation:
- Physical therapy sessions: $50 – $150 per session (usually 5-10 sessions)
Robot-Assisted Hip Replacement
Definition and Details:
Robot-Assisted Hip Replacement is a cutting-edge surgical technique that utilizes robotic technology to enhance precision and improve outcomes during hip replacement surgeries.
The robot assists the surgeon in accurately positioning the implants, resulting in more favorable alignment and improved stability.
This method is particularly beneficial for patients with complex anatomical considerations or those requiring revision surgeries.
Robot-assisted procedures typically offer benefits such as reduced postoperative pain, shorter hospital stays, and quicker recovery times.
Procedure Steps:
- Preoperative Assessment: Thorough evaluation and imaging studies to assess hip condition.
- Anesthesia Administration: General or regional anesthesia is administered.
- Incision and Exposure: A small incision is made to access the hip joint.
- Robotic Guidance Setup: The robotic system is calibrated based on preoperative imaging to assist during the surgery.
- Removal of Damaged Joint: The damaged femoral head and acetabulum are excised.
- Insertion of Prosthesis with Robot Assistance: The robotic system aids in precise placement of the prosthesis.
- Closure of the Incision: The incision is closed with sutures or staples.
- Postoperative Recovery: Monitoring and initiation of physical therapy.
Pricing Breakdown:
Preoperative Assessments:
- X-rays: $100 – $300
- MRI (if needed): $500 – $1,200
- Blood tests: $100 – $200
Surgical Costs:
- Surgeon’s fee: $2,500 – $4,500
- Anesthesiologist’s fee: $600 – $1,200
- Robot-assisted prosthesis implant: $6,000 – $12,000
Hospitalization:
- Daily hospital stay: $600 – $1,800 per day (typically 1-3 days)
- Nursing care and monitoring: $200 – $500 per day
Rehabilitation:
- Physical therapy sessions: $50 – $150 per session (usually 5-10 sessions)
Hip Replacement with Stem Cells
Definition and Details:
Hip Replacement with Stem Cells is an innovative procedure that combines traditional hip replacement techniques with stem cell therapy to enhance healing and recovery.
This approach involves the use of the patient’s own stem cells, which are harvested and injected into the surgical site during the procedure.
The goal is to promote tissue regeneration, reduce inflammation, and improve overall outcomes. This technique is still relatively new and may not be widely available in all surgical centers.
Procedure Steps:
- Preoperative Assessment: Evaluation of the hip condition and imaging studies.
- Stem Cell Harvesting: Stem cells are collected from the patient’s fat or bone marrow.
- Anesthesia Administration: General or regional anesthesia is administered.
- Incision and Exposure: A surgical incision is made to access the hip joint.
- Removal of Damaged Joint: The damaged femoral head and acetabulum are removed.
- Insertion of Prosthesis: The artificial components are implanted.
- Injection of Stem Cells: The harvested stem cells are injected into the surgical site.
- Closure of the Incision: The incision is closed with sutures or staples.
- Postoperative Recovery: Monitoring and initiation of physical therapy.
Pricing Breakdown:
Preoperative Assessments:
- X-rays: $100 – $300
- MRI (if needed): $500 – $1,200
- Blood tests: $100 – $200
Surgical Costs:
- Surgeon’s fee: $2,500 – $4,500
- Anesthesiologist’s fee: $600 – $1,200
- Stem cell harvesting and processing: $1,000 – $3,000
- Hip prosthesis implant: $4,000 – $9,000
Hospitalization:
- Daily hospital stay: $600 – $1,800 per day (typically 1-2 days)
- Nursing care and monitoring: $200 – $500 per day
Rehabilitation:
- Physical therapy sessions: $50 – $150 per session (usually 5-10 sessions)
QUICK, 100% FREE ONLINE QUOTE
Additional Considerations: Making an Informed Choice
While the cost is a significant factor in deciding to undergo a total hip prosthesis, other elements should also be considered:
Quality of Care
Turkey has established itself as a medical tourism hub, with many hospitals accredited by international organizations such as JCI (Joint Commission International). Look for facilities with experienced orthopedic surgeons, high success rates, and positive patient testimonials.
Language Barrier
If you are traveling to Turkey from abroad, consider facilities that offer multilingual staff or international patient coordinators to assist you throughout the process.
This can greatly enhance your overall experience and help mitigate any misunderstandings.
Travel and Accommodation Costs
If you are traveling to Turkey for your procedure, factor in the costs of flights, accommodations, and meals. Depending on your travel plans, this could add an additional $1,000 to $3,000 to your overall expenses.
Insurance Coverage
Check with your health insurance provider to see if they cover international medical expenses. Some plans may offer partial coverage for procedures done overseas, which can significantly reduce your out-of-pocket expenses.
Follow-Up Care
Postoperative follow-up is crucial to ensure proper healing and function of the new hip joint. This may involve additional visits to the surgeon or physical therapist, which can incur extra costs.
How to prepare for a Total hip prosthesis procedure?
Personal Preparations
Educate Yourself:
- Research the Procedure: Understanding the intricacies of hip replacement surgery, including the types of implants available, the surgical techniques used, and the expected outcomes, can ease anxiety and help you make informed decisions. Read reputable sources, watch videos, and join support groups to gather insights from others who have undergone the surgery.
- Understand Recovery: Familiarize yourself with the recovery timeline, including potential challenges and milestones. Knowing what to expect can mentally prepare you for the journey ahead.
Discuss with Your Family:
- Communicate Your Plans: Inform your family about your surgery date, recovery needs, and how they can support you. Having a solid support system can make a significant difference in your emotional well-being and physical recovery.
- Arrange for Assistance: Plan for someone to help you with daily activities like cooking, cleaning, and grocery shopping during the initial recovery phase. This will allow you to focus on healing without overwhelming yourself.
Adopt a Healthy Lifestyle:
- Eat Nutritiously: Prioritize a balanced diet rich in vitamins, minerals, and protein to promote healing. Incorporate fruits, vegetables, lean proteins, and whole grains into your meals. Avoid processed foods and excessive sugar, as these can slow recovery.
- Stay Hydrated: Drinking plenty of water is crucial before surgery. Staying hydrated helps maintain optimal body functions, aids digestion, and supports overall health.
Maintain Physical Activity:
- Strengthening Exercises: Engage in low-impact exercises, such as swimming or cycling, to strengthen the muscles around your hip joint. Consult with your doctor or physical therapist to establish a safe exercise plan tailored to your needs.
- Practice Mobility: Use walking aids, like a cane or walker, to practice mobility and improve your balance. This can boost your confidence and prepare you for post-surgery movement.
Adjust Your Living Space:
- Create a Safe Environment: Make your home safe and comfortable for recovery by removing tripping hazards (like loose rugs and clutter) and ensuring adequate lighting. Consider arranging essential items within easy reach to minimize movement.
- Organize a Recovery Zone: Set up a designated area in your home with a comfortable chair, pillows, and entertainment options (books, TV, etc.) to facilitate rest during your recovery period.
Stop Smoking:
- Quit Smoking: If you smoke, consider quitting before your surgery. Smoking can impede healing and increase the risk of complications. Seek support from healthcare providers or cessation programs to assist in your quit journey.
- Avoid Alcohol: Reduce or eliminate alcohol intake as it can interfere with anesthesia and medication effectiveness, as well as hinder the healing process.
Plan Your Medications:
- Review Current Medications: Create a list of all medications you take, including prescriptions, over-the-counter drugs, and supplements. Discuss this list with your doctor to identify any that may need to be adjusted or paused before surgery.
- Organize Pain Management: Talk with your doctor about pain management options post-surgery. Understanding the types of medications and their timing can alleviate anxiety and help with your recovery plan.
Mental Preparation:
- Manage Expectations: Recognize that recovery is a gradual process that requires patience. Set realistic goals and celebrate small achievements along the way to maintain motivation.
- Practice Relaxation Techniques: Incorporate practices like meditation, deep breathing exercises, or yoga to reduce anxiety and enhance your emotional state before surgery.
Financial Preparation:
- Understand Costs: Review your health insurance coverage and estimate out-of-pocket expenses for the procedure, rehabilitation, and any potential complications. Knowing your financial responsibilities can alleviate stress.
- Budget for Recovery: Consider setting aside funds for any necessary home modifications, medications, or assistive devices you might need post-surgery.
Prepare for the Day of Surgery:
- Pack Your Hospital Bag: Create a list of items to bring to the hospital, such as comfortable clothing, toiletries, personal identification, insurance documents, and any items that can enhance your comfort (like a book or tablet).
- Plan Transportation: Arrange for someone to drive you to and from the hospital, as you will not be able to drive yourself post-surgery due to anesthesia effects.
Preparations with Your Doctor
Schedule Preoperative Appointments:
- Comprehensive Evaluation: Attend all scheduled appointments to allow your doctor to assess your health status and readiness for surgery. This may include blood tests, imaging studies (like X-rays or MRIs), and physical exams to evaluate your overall fitness.
- Discuss Medical History: Provide your doctor with a complete medical history, including any chronic conditions, allergies, or previous surgeries. This information is crucial for tailoring your anesthesia and surgical plan.
Clear Communication:
- Discuss Concerns and Questions: Prepare a list of questions regarding the procedure, recovery, and any concerns you may have. A clear understanding can enhance your confidence and reduce anxiety.
- Understand the Risks: Have an open conversation with your surgeon about potential risks and complications associated with hip replacement surgery, as well as how they are managed.
Confirm Surgical Details:
- Review Surgical Plan: Go over the specifics of the surgical plan, including the type of implant to be used, the surgical technique, and the estimated duration of the procedure. Ensure you feel comfortable with the approach.
- Understand Anesthesia Options: Discuss anesthesia choices (general vs. regional) and understand what to expect during and after the administration.
Preoperative Instructions:
- Follow Dietary Guidelines: Adhere to any dietary restrictions your doctor provides, such as fasting requirements before surgery. This is crucial for a safe anesthesia process.
- Medications Guidance: Follow your doctor’s instructions regarding medications. Some may need to be stopped or adjusted before surgery, such as blood thinners or anti-inflammatory drugs.
Coordinate Rehabilitation Plans:
- Discuss Physical Therapy: Talk about the rehabilitation plan, including the type of physical therapy recommended after surgery. Understanding this process can motivate you to stay committed to your recovery.
- Set Recovery Goals: Work with your healthcare team to establish realistic goals for your rehabilitation journey.
Review Postoperative Care:
- Understand Aftercare Requirements: Discuss the aftercare process, including wound care, signs of infection, and when to seek medical help. Knowing what to look for can ease anxiety post-surgery.
- Pain Management Strategies: Go over your pain management plan, including prescribed medications, dosages, and any alternative pain relief options that might be recommended.
Update Health Records:
- Ensure Accurate Records: Provide your doctor with any updates regarding your health status or changes in medications to ensure your records are up-to-date before the procedure.
- Check Vaccination Status: Ensure your vaccinations are current, especially for conditions like pneumonia and influenza, to reduce post-surgery complications.
Identify Support Resources:
- Discuss Available Resources: Ask your doctor about support resources, including rehabilitation centers, home health services, and community support groups for post-surgery assistance.
- Referral to Specialists: If needed, obtain referrals to specialists, such as physical therapists or pain management experts, to help in your recovery.
Finalize Surgical Consent:
- Understand the Consent Process: Be prepared to sign a consent form prior to surgery. Ensure you understand the information within the consent, and ask questions if anything is unclear.
- Verify Surgical Site: Confirm the surgical site and procedure with your healthcare team on the day of surgery to avoid any mistakes.
Logistics and Transportation:
- Discuss Hospital Arrival Times: Verify what time you should arrive at the hospital for preoperative preparations. This may include any required tests or assessments before the procedure.
- Arrange for Discharge Plans: Talk about what your discharge plan will look like, including follow-up appointments and any needed home health care services.
What happens during a Total hip prosthesis procedure?
Anesthesia Administration
Before the surgery begins, the patient is prepared for anesthesia.
What the Doctor Does:
- Evaluates the patient’s medical history and current health status to determine the appropriate anesthesia method (general or regional).
- Administers the chosen anesthesia via an IV or spinal injection.
- Monitors the patient’s vital signs (heart rate, blood pressure, oxygen levels) to ensure safety throughout the procedure.
Surgical Site Preparation
Once the anesthesia takes effect, the surgical area is cleaned and prepared.
What the Doctor Does:
- Shaves and cleans the area around the hip to minimize the risk of infection.
- Applies antiseptic solutions to disinfect the surgical site.
- Places sterile drapes around the area to create a sterile field.
Incision
The surgeon makes an incision to access the hip joint.
What the Doctor Does:
- Chooses the incision site based on the surgical approach (anterior, posterior, or lateral).
- Utilizes a scalpel to carefully cut through the skin and underlying tissues, including muscles and fascia.
- Ensures minimal damage to surrounding tissues to promote faster healing.
Exposing the Joint
The surgeon carefully exposes the hip joint by retracting surrounding muscles and tissues.
What the Doctor Does:
- Utilizes retractors to hold back muscles and tissues, providing a clear view of the hip joint.
- Identifies and preserves important structures, such as blood vessels and nerves, during this process.
- Takes necessary measures to minimize bleeding and maintain a clear surgical field.
Removal of Damaged Bone and Cartilage
The damaged parts of the hip joint are removed to prepare for the prosthesis.
What the Doctor Does:
- Uses specialized instruments to excise the femoral head (the ball of the hip joint) and any damaged cartilage from the acetabulum (the socket).
- Evaluates the remaining bone for any irregularities or additional damage that may require treatment.
- Measures the bone to ensure proper sizing of the prosthetic components.
Preparation of the Acetabulum
The acetabulum is shaped and prepared to fit the new implant.
What the Doctor Does:
- Uses reamers (surgical instruments) to smooth and shape the acetabulum to accommodate the prosthetic socket.
- Ensures the implant will fit securely within the socket, optimizing stability and longevity.
- May use bone cement or press-fit techniques to secure the implant, depending on the type of prosthesis being used.
Insertion of the Acetabular Component
The socket component of the hip prosthesis is inserted into the acetabulum.
What the Doctor Does:
- Positions the acetabular implant into the prepared socket, ensuring proper alignment and stability.
- Uses a hammer or impactor to gently tap the implant into place, ensuring a secure fit.
- Checks the alignment and stability of the component before proceeding to the femoral component.
Preparation of the Femur
The femur is prepared for the insertion of the prosthetic femoral component.
What the Doctor Does:
- Uses an osteotomy (bone-cutting) technique to create a cavity in the femur for the prosthetic stem.
- Ensures the femur is properly sized and shaped to accommodate the new implant.
- Checks for proper fit and stability to prevent complications during recovery.
Insertion of the Femoral Component
The prosthetic stem is inserted into the femur.
· What the Doctor Does:
- Positions the femoral implant into the cavity created in the femur.
- Ensures that the prosthesis is correctly aligned with the acetabular component to provide optimal joint movement.
- Secures the implant using bone cement (if applicable) or utilizes a press-fit technique for stability.
Closing the Incision
Once the implants are securely in place, the surgical site is closed.
What the Doctor Does:
- Carefully repositions any muscles and tissues that were retracted during the procedure.
- Sutures or staples the layers of tissue back together, starting with the deep tissues and finishing with the skin.
- Applies a sterile dressing to the incision site to protect it during the initial healing phase.
What happens after a Total hip prosthesis procedure?
Immediate Post-Operative Care
Hospital Stay
Following the surgery, patients are typically monitored in a recovery room for several hours before being moved to a hospital room.
This initial stage involves:
- Monitoring Vital Signs: Healthcare providers will closely observe vital signs such as heart rate, blood pressure, and oxygen levels to ensure the patient is stable.
- Pain Management: The medical team will administer medications to manage pain effectively, often using a combination of opioids and non-opioid analgesics. Patients are encouraged to communicate their pain levels regularly.
- Infection Prevention: Antibiotics may be given to minimize the risk of infection. The surgical site will be kept clean and monitored for any signs of complications.
Mobility and Rehabilitation
Within the first 24 hours after surgery, physical therapy usually begins. This is a crucial part of recovery:
- Physical Therapy: A physical therapist will guide patients through gentle range-of-motion exercises and teach them how to safely get in and out of bed and use mobility aids like walkers or crutches.
- Weight-Bearing Activity: Depending on the surgeon’s protocols, patients may be allowed to begin bearing weight on the operated leg shortly after surgery, sometimes as early as the next day. This gradual introduction to weight-bearing helps to prevent stiffness and promotes circulation.
Short-Term Healing Period (First Few Weeks)
Hospital Discharge
Patients generally stay in the hospital for 2 to 5 days, depending on their overall health and how well they recover. Before discharge, healthcare providers will ensure:
- Satisfactory Pain Control: Patients should be able to manage pain with oral medications before going home.
- Understanding Care Instructions: Patients receive instructions on wound care, medication management, and signs of complications that should prompt immediate medical attention.
Home Care
Once discharged, patients continue their recovery at home with a focus on:
- Wound Care: Patients must keep the surgical site clean and dry. Regular dressing changes and monitoring for redness, swelling, or drainage are essential to prevent infection.
- Pain Management: It is vital to continue prescribed pain medications as needed. Patients should also be aware of any side effects and communicate with their healthcare providers.
- Physical Activity: Patients are encouraged to continue physical therapy exercises at home as instructed. Gradually increasing mobility helps in regaining strength and flexibility.
Follow-Up Appointments
Patients will have follow-up visits with their orthopedic surgeon within 1 to 2 weeks after surgery to assess:
- Wound Healing: The surgeon will examine the incision site for proper healing and signs of infection.
- Range of Motion and Strength: The surgeon will evaluate the patient’s progress and adjust rehabilitation plans as necessary.
Long-Term Healing Period (Weeks to Months)
Rehabilitation
The long-term recovery phase typically spans several months, with specific milestones in physical rehabilitation:
- Continued Physical Therapy: Rehabilitation often continues for 6 to 12 weeks post-surgery. Patients may attend outpatient therapy sessions focusing on strengthening exercises, balance training, and walking techniques.
- Home Exercise Program: A home exercise regimen is developed to promote ongoing improvement in strength and mobility. Patients should follow the therapist’s guidance to ensure safe progression.
Activities of Daily Living
As recovery progresses, patients gradually return to their normal activities, but adaptations may be necessary:
- Resuming Daily Activities: Patients are encouraged to gradually resume daily activities, such as bathing, dressing, and light household chores, as tolerated.
- Avoiding High-Impact Activities: High-impact activities or sports should be avoided for at least 3 to 6 months. Patients should consult their healthcare provider for personalized recommendations based on their recovery.
Monitoring for Complications
During the long-term recovery phase, patients should remain vigilant for potential complications:
- Signs of Infection: Any increase in pain, swelling, fever, or unusual discharge from the surgical site warrants immediate medical evaluation.
- Blood Clots: Patients should be aware of symptoms such as swelling, redness, or pain in the legs, which could indicate a deep vein thrombosis (DVT).
- Prosthesis Issues: Although rare, issues with the prosthesis, such as loosening or dislocation, can occur. Patients should report any unusual sensations or limitations in movement.
Emotional and Psychological Recovery
In addition to physical healing, the emotional and psychological aspects of recovery are equally important:
- Support Systems: Engaging family and friends for support during the recovery process can improve emotional well-being. Patients may benefit from discussions about their experiences and challenges.
- Counseling and Support Groups: Some patients may find it helpful to speak with a counselor or join support groups for individuals undergoing similar experiences, providing a space for shared stories and encouragement.
Final Recovery Assessment
Typically, full recovery can take anywhere from 3 to 12 months. Patients will have a final follow-up appointment with their orthopedic surgeon during this period to:
- Assess Overall Recovery: The surgeon will evaluate the functionality of the hip, including range of motion and strength.
- Discuss Long-Term Care: Patients will receive advice on long-term joint health, including weight management, exercise routines, and lifestyle changes to enhance their quality of life.
The Final Takeaway.
Undergoing a total hip prosthesis is a major decision that can significantly impact your quality of life. Turkey offers a wealth of options for patients seeking this procedure, with affordable costs and high-quality care.
By carefully considering all aspects of pricing and preparing for your journey, you can ensure a smoother experience and a successful return to an active lifestyle.

